Featured Articles

Dealing With Blisters on the Feet

Dealing with blisters on your feet can be quite uncomfortable, but with proper care, you can find relief and avoid potential complications. It's essential to first identify the underlying cause of your blister. They often develop from friction or pressure on the skin, typically caused by ill-fitting shoes, high heels, or excessive moisture. Maintaining good hygiene is important when dealing with blisters. Cleanse the affected area gently with mild soap and water. Avoid the temptation to pop the blister, as this can introduce infection and slow down the healing process. To alleviate discomfort and protect the blister, consider using specialized blister pads or moleskin. These materials can reduce friction and provide cushioning, making it easier for the blister to heal. Choosing appropriate footwear is essential for blister prevention. Opt for shoes that fit well and are made of breathable materials to minimize friction and moisture buildup. Wearing moisture-wicking socks, applying lubricants like petroleum jelly, or using insoles for added cushioning can help prevent blisters from forming. If your blisters persist, worsen, or become infected, it's suggested that you make an appointment with a podiatrist who can provide the proper care for your feet.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
Tips for a Speedy Recovery From a Broken Toe

A broken toe can be a painful and inconvenient injury, but with proper care, you can help it heal more quickly and minimize discomfort. First and foremost, it is essential to rest and protect the injured toe. This means avoiding putting weight on it and wearing comfortable, supportive footwear. Swelling and pain can be reduced by elevating the foot whenever possible, and taking over-the-counter pain relievers may provide some relief. In some cases, a splint or buddy taping the broken toe to its neighbor toe can aid in stabilization. Be mindful of any signs of infection, such as increased pain, redness, or discharge, and seek medical attention promptly if you notice these symptoms. Patience is key when caring for a broken toe, as it may take several weeks to fully heal. If you have broken your toe, it is suggested that you contact a podiatrist who can accurately diagnose this condition, and guide you toward the treatment that is right for you.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
Trauma to the foot, especially the toes, can occur in many ways. Banging them, stubbing them, or dropping something on them are a few different ways this trauma can occur. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break or fracture. Another type of trauma that can break a toe is repeated activity that places stress on the toe for prolonged periods of time.
Broken toes can be categorized as either minor or severe fractures. Symptoms of minor toe fractures include throbbing pain, swelling, bruising on the skin and toenail, and the inability to move the toe with ease. Severe toe fractures require medical attention and are indicated when the broken toe appears crooked or disfigured, when there is tingling or numbness in the toe, or when there is an open, bleeding wound present on the toe.
Generally, a minor toe break will heal without long-term complications. However, it is important to discontinue activities that put pressure on the toe. It is best to stay off of the injured toe and immediately get a splint or cast to prevent any more additional movement of the toe bones. You can also immobilize your toe by placing a small cotton ball between the injured toe and the toe beside it. Then, tape the two toes together with medical tape. Swelling can be alleviated by placing an ice pack on the broken toe directly as well as elevating your feet above your head.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery, especially when the big toe has been broken. Due to its position and the pressure the big toe endures with daily activity, future complications can occur if it is not properly treated. Pain associated with minor toe fractures can be managed with over-the-counter pain medications. Prescription pain killers may be necessary for severe toe fractures.
The healing time for a broken toe is approximately four to six weeks. In severe cases where the toe becomes infected or requires surgery, healing time can take up to eight weeks or more. While complications associated with a broken toe are immediately apparent, it is important to note that there are rare cases when additional complications, such as osteoarthritis, can develop over time. You should immediately speak with your podiatrist if you think you have broken your toe due to trauma. They will be able to diagnose the injury and recommend the appropriate treatment options.
Arthritis Can Cause Pain in the Feet and Ankles
The Job Description of a Podiatrist

Podiatrists, often referred to as foot doctors, are healthcare professionals specializing in the diagnosis, treatment, and prevention of disorders and injuries related to the feet and ankles. Their job entails a diverse range of responsibilities to ensure optimal foot health for their patients. Podiatrists conduct thorough examinations to diagnose various foot conditions, including bunions, plantar fasciitis, and diabetic foot ulcers. They often use diagnostic tools such as X-rays and laboratory tests to aid in their assessments. Once a diagnosis is made, podiatrists develop individualized treatment plans, which may involve prescribing medications or performing surgical procedures. Additionally, podiatrists educate patients on proper foot care, footwear, and prevention strategies. They may also collaborate with other healthcare professionals to address underlying health conditions that affect the feet, such as diabetes or arthritis. In addition to clinical work, some podiatrists conduct research to advance the field's knowledge and develop innovative treatments. Overall, podiatrists are dedicated to improving the quality of life for individuals by ensuring the health and functionality of their feet and lower limbs. If you are interested in pursuing a career in podiatry, it is strongly suggested that you speak to this type of doctor who can provide you with valuable information.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
The branch of medicine that is focused on the treatment, diagnosis, and study of disorders of the lower leg, ankle and foot is referred to as podiatry. Because people often spend a great deal of their time on their feet, many problems in this area can occur. A person seeks help from the field of podiatry when they need treatment for heel spurs, bunions, arch problems, deformities, ingrown toenails, corns, foot and ankle problems, infections, and problems with the foot that are related to diabetes and additional diseases.
To treat problems of the foot, ankle or lower leg, a podiatrist may prescribe physical therapy, drugs, perform surgery, or set fractures. Individuals may also be recommended to wear corrective shoe inserts, custom-made shoes, plaster casts and strappings in order to correct deformities.
When trying to gather information on a patient problem, a scanner or force plate may be used in order to design orthotics. During this procedure, patients are told to walk across a plate that is connected to a computer; the computer then takes a scan of the foot and indicates weight distribution and pressure points. The computer readouts will give the podiatrist information to help them determine the correct treatment plans.
Diagnosis is also provided through laboratory tests and x-rays. Through the foot, the first signs of serious problems such as heart disease, diabetes and arthritis can show up. For example, individuals that have diabetes may frequently have problems such as infections and foot ulcers because they experience poor circulation in the foot area. A podiatrist can then have consultations with patients when symptoms arise. Referrals will then be made to specialists that handle the greater health problems.
Some podiatrists have their own independent, private practices or clinics where they have a small staff and administrative personnel. Many podiatrists work within group practices. They usually spend time performing surgery in ambulatory surgical centers or hospitals, or visit patients in nursing homes. Podiatrists typically spend between 30 to 60 hours of week working. Some podiatrists specialize in public health, orthopedics, surgery, or primary care. Other fields include specialties in geriatrics, dermatology, pediatrics, diabetic foot care and sports medicine.
Some podiatrist specialists complete extra training in the area of foot and ankle reconstruction that results from the effects of physical trauma or diabetes. There are also surgeons that perform surgery of a cosmetic nature to correct bunions and hammertoes.
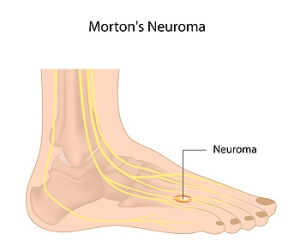
Facts About Morton’s Neuroma
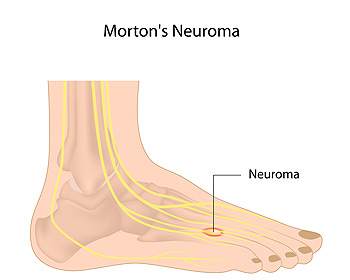
Morton's neuroma is a relatively common but often misunderstood foot condition that can lead to discomfort and pain. This condition can be demystified by exploring essential facts about Morton's neuroma. Morton's neuroma typically occurs between the third and fourth toes, though it can develop in other spaces in the foot. Despite its name, Morton's neuroma is not a tumor. It is actually a thickening of the tissue surrounding the nerves leading to the toes. Common symptoms can include sharp, burning pain or the sensation of a pebble in the shoe, typically while walking or running. Morton’s neuroma can be triggered by wearing tight shoes, high heels, or activities that put repetitive pressure on the forefoot, such as running. Treatment of Morton's neuroma can be managed with conservative measures such as wearing wider shoes, or using cushioned insoles. If conservative treatments do not provide relief, surgical removal of the neuroma may be considered. Effective preventive measures include wearing proper footwear, maintaining a healthy weight, and addressing foot issues promptly. If you have any of these symptoms, it is suggested that you consult a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Causes and Solutions for Second Toe Pain

Second toe pain can be a bothersome and discomforting issue, impacting your daily activities and quality of life. Understanding the potential causes and effective treatments is crucial for finding relief and maintaining optimal foot health. One common culprit of second toe pain is wearing improperly fitting shoes. Tight, narrow, or pointy shoes can compress the toes, leading to discomfort and deformities such as hammertoes. High heels, which force excessive weight onto the toes, can exacerbate this problem. Another frequent cause is overuse or repetitive stress, often seen in athletes or individuals engaged in activities that involve pushing off with the toes. This can lead to conditions that can include metatarsalgia or stress fractures. To address second toe pain, begin by wearing comfortable, properly fitting shoes with adequate toe room. Wearing custom orthotics can provide additional support and alleviate pressure. Rest, and taking over-the-counter pain relievers can help manage acute pain, and exercises may be beneficial for chronic issues. If second toe pain persists or worsens, it is suggested that you consult a podiatrist for a proper diagnosis and tailored treatment plan.
Toe pain can disrupt your daily activities. If you have any concerns, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.