Featured Articles

Soccer and Ankle Injuries

Ankle injuries are a frequent occurrence in the high-paced world of soccer, posing challenges for players of all levels. The nature of the sport, characterized by sudden changes in direction, rapid acceleration, and physical contact, makes ankles vulnerable to sprains, strains, and fractures. One common injury is the ankle sprain, which occurs when the ligaments supporting the joint are stretched or torn, often due to a sudden twist or roll of the foot. Another concern is ankle fractures, which involve a break in one or more bones in the ankle joint and can result from direct trauma or excessive force. These injuries not only cause pain and swelling but also disrupt player performance and sideline athletes for weeks or even months. Preventive measures such as proper warm-up routines, wearing supportive footwear, and practicing techniques for safe landing and pivoting can help reduce the risk of ankle injuries. If have sustained an ankle injury while playing soccer, it is suggested that you promptly consult a podiatrist for effective treatment solutions.
Ankle and foot injuries are common among athletes and in many sports. They can be caused by several problems and may be potentially serious. If you are feeling pain or think you were injured in a sporting event or when exercising, consult with one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Common Injuries
The most common injuries that occur in sporting activities include:
- Achilles Tendonitis
- Achilles Tendon Rupture
- Ankle Sprains
- Broken Foot
- Plantar Fasciitis
- Stress Fractures
- Turf Toe
Symptoms
Symptoms vary depending upon the injury and in some cases, there may be no symptoms at all. However, in most cases, some form of symptom is experienced. Pain, aching, burning, bruising, tenderness, tightness or stiffness, sensation loss, difficulty moving, and swelling are the most common symptoms.
Treatment
Just as symptoms vary depending upon the injury, so do treatment options. A common treatment method is known as the RICE method. This method involves rest, applying ice, compression and elevating the afflicted foot or ankle. If the injury appears to be more serious, surgery might be required, such as arthroscopic or reconstructive surgery. Lastly, rehabilitation or therapy might be needed to gain full functionality in the afflicted area. Any discomfort experienced by an athlete must be evaluated by a licensed, reputable medical professional.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Sports Related Foot and Ankle Injuries
Foot and ankle injuries are common among athletes and those who exercise frequently. Most of these injuries are non-life-threatening and can heal in weeks with proper treatment and care. Serious injuries, however, require urgent medical treatment.
Common minor injuries include ankle sprains, ankle strains, Achilles tendonitis, plantar fasciitis, stress fractures, and turf toe. An ankle sprain is when the ligaments in the ankle have either become stretched or torn. When the muscle or tendon is stretched or torn, it is an ankle strain. When the big toe is sprained, it is known as turf toe. Achilles tendonitis is the overuse and inflammation of the Achilles tendon. Plantar fasciitis is the inflammation of the plantar fascia and generally occurs from overuse in athletics. Stress fractures are also caused from overuse and are small cracks in the bone.
Achilles tendon ruptures are common, but more serious. This injury occurs when the Achilles tendon, the largest tendon in the body, ruptures. In most cases, this causes severe pain and difficulty walking; some who have experienced this injury have reported, however, no signs or symptoms. A laceration is a deep cut that can occur anywhere on the body. Lacerations on the foot are rarer, but can occur from things like metal cleats landing on the foot.
Treatment options cover a wide range of methods based upon the injury and its severity. Conditions like plantar fasciitis, stress fractures, Achilles tendonitis, turf toe and ankle sprains/ strains can heal on their own without immediate medical care, but seeing a podiatrist to monitor the injury is always recommended. Following the RICE (Rest, Icing, Compression, and Elevation) protocol is generally enough to treat minor injuries. This means resting the foot by either keeping pressure off the foot or not walking at all. Icing the injury will help reduce swelling and pain. Compressing the wound with a wrap will immobilize and help promote healing. Finally, keeping the wound elevated will also reduce swelling and also help the healing process.
It is important to note that even minor injuries can vary in severity, with grade one being a minor injury and grade three requiring urgent care by a podiatrist. Achilles tendon ruptures and lacerations on the foot generally require urgent medical care and treatment options that need a podiatrist. These could include imaging tests, stitches for cuts, rehabilitation, and casts or braces. Every case is different, however, so it is always recommended to see a podiatrist when pain in the foot does not disappear.
Causes and Treatment of Plantar Fasciitis

Plantar fasciitis, an inflammation of the plantar fascia, often affects individuals between 40-60 years old. This is due to factors like excessive pronation, high arches, or prolonged standing that affect the broad band of tissue that runs along the bottom of the foot. One of the main symptoms of plantar fasciitis is sharp heel pain, particularly in the morning or after rest, which can radiate along the foot's arch. Initial management of plantar fasciitis may involve reducing inflammation and pain by moderating activity, taking certain pain relievers, and wearing properly fitting shoes. A podiatrist can assess factors like foot structure, gait abnormalities, and muscle imbalances that may contribute to the condition. Physiotherapy with stretching and strengthening exercises also may be implemented. A podiatrist may recommend advanced treatments like corticosteroid injections for persistent symptoms. In severe cases, podiatric surgical options, such as plantar fasciotomy, may be considered. It is suggested that you make an appointment with a podiatrist, who can conduct a thorough exam and suggest the best treatment options for plantar fasciitis discomfort.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Why Live with Pain and Numbness in Your Feet?
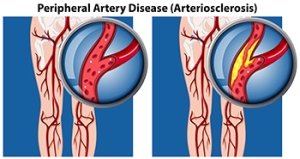
How Peripheral Artery Disease Affects the Feet
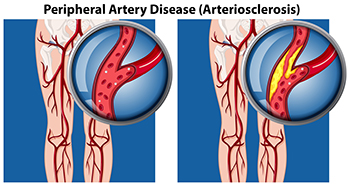
Peripheral artery disease, or PAD, affects millions of individuals in the United States. It is caused by reduced blood flow due to plaque buildup in peripheral arteries. PAD often targets the lower extremities, seriously affecting the legs and feet. A common indicator of peripheral artery disease is intermittent muscle pain in the lower legs during activity that subsides with rest. Other signs include diminished toenail and leg hair growth, temperature disparities between feet and non-healing wounds. Treatment from a podiatrist is essential for alleviating symptoms and preventing further complications. Podiatrists can offer various treatment options for PAD, including custom orthotic devices and footwear modifications, and in severe cases, surgical intervention. Additionally, lifestyle adjustments, such as smoking cessation and managing underlying conditions like hypertension, are essential in PAD management. Early intervention not only improves quality of life but also reduces the risk of severe complications associated with PAD. If you experience symptoms of peripheral artery disease that is affecting your lower legs and feet, it is suggested that you schedule an appointment with a podiatrist.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Origins of Blisters on the Feet

Blisters on the feet can be an unwelcome nuisance, often causing discomfort and hindering mobility. These fluid-filled sacs typically form in response to friction or repetitive rubbing against the skin. When excessive pressure or irritation occurs, the outer layer of the skin separates from the underlying tissue, creating a protective bubble filled with fluid. Common culprits behind blister formation include wearing ill-fitting shoes, prolonged periods of walking or running, and friction caused by sweaty or damp conditions. Additionally, certain activities, such as hiking or wearing new shoes without proper breaking in, can increase the likelihood of developing blisters. Individuals with foot deformities or abnormalities may also be more prone to blister formation due to uneven pressure distribution. If you have a blister on your foot that has become infected, it is suggested that you consult a podiatrist who can safely treat it and provide effective prevention techniques for future knowledge.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
Causes of Foot Swelling
 Swelling in the feet, otherwise known as edema, has a range of mild to severe causes. Mild edema may result from standing or sitting for long periods, especially in hot weather. This causes fluid to pool in the lower extremities. Swelling can also be a side effect of certain medications, hormonal changes, or dietary factors like excessive salt intake. In more severe cases, edema may be a sign of underlying medical conditions, such as heart failure, kidney disease, or venous insufficiency. In these cases, the body’s fluid balance is off, leading to fluid retention and swelling in the feet and ankles. Certain injuries, infections, or blood clots in the legs can also cause localized edema. Podiatrists, or foot doctors, can diagnose the underlying cause of foot swelling. They may recommend lifestyle modifications, compression therapy, medication management, or other treatments to address the cause. If you have swelling in the feet or ankles, it is suggested that you make an appointment with a podiatrist to find relief.
Swelling in the feet, otherwise known as edema, has a range of mild to severe causes. Mild edema may result from standing or sitting for long periods, especially in hot weather. This causes fluid to pool in the lower extremities. Swelling can also be a side effect of certain medications, hormonal changes, or dietary factors like excessive salt intake. In more severe cases, edema may be a sign of underlying medical conditions, such as heart failure, kidney disease, or venous insufficiency. In these cases, the body’s fluid balance is off, leading to fluid retention and swelling in the feet and ankles. Certain injuries, infections, or blood clots in the legs can also cause localized edema. Podiatrists, or foot doctors, can diagnose the underlying cause of foot swelling. They may recommend lifestyle modifications, compression therapy, medication management, or other treatments to address the cause. If you have swelling in the feet or ankles, it is suggested that you make an appointment with a podiatrist to find relief.
Swollen feet can be a sign of an underlying condition. If you have any concerns, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Swollen feet are a common ailment among pregnant women and people who stand or sit for extended periods. Aging may increase the possibility of swollen feet and patients who are obese often notice when their feet are swelling too. There may be medical reasons why swollen feet occur:
- Phlebitis - A condition that causes the veins to become inflamed and can also cause leg pain.
- Liver disease - This may lead to low blood levels of albumin which is a protein. This can cause fluid in the blood to pass into the tissues and several areas of the body can become swollen.
- Heart failure - When the heart doesn’t pump properly the blood that is normally pumped back to the heart can pool in the veins of the legs causing swollen feet.
- Kidney disease - One of the main functions of the kidneys is releasing excess fluid in the body. This type of condition can make it difficult for the kidneys to function properly, and as a result the feet may become swollen.
- Deep-vein thrombosis (DVT)- This is a serious condition where blood clots form in the veins of the legs. They can block the return of blood from the legs to the heart which may cause the feet to swell. It is important to be treated by a podiatrist if this condition is present.
Swollen feet can also be caused by bone and tendon conditions, including fractures, arthritis, and tendinitis. Additionally, there may be skin and toenail conditions and an infection may cause the feet to swell. Patients who take medicine to treat high blood pressure may be prone to getting swollen feet.
Many patients elevate their feet to help relieve the swelling and this is generally a temporary remedy. When a podiatrist is consulted the reason behind the swelling can be uncovered and subsequently treated.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.