Blog

Is Surgery Necessary to Treat Stress Fractures?

A stress fracture is a hairline fracture that commonly happens in the foot and may be prevalent among people who enjoy running. It occurs as a result of repeated stress the foot endures from physical activity, and the pain can gradually worsen if it is not treated promptly. It is suggested to temporarily cease the activity that caused the fracture, and relief may come from frequently elevating and resting the foot. Research has shown that people who are deficient in vitamin D or calcium may be susceptible to getting stress fractures, and it is advised to increase these types of supplements, if applicable. Additionally, when crutches are used, healing may be accelerated as the weight is kept off of the affected foot. If the fracture is severe, surgery may be necessary for permanent healing. The full recovery period for stress fracture surgery can be up to eight weeks, and low-impact activities can be performed as the healing takes place. If you think you may have a stress fracture, please consult with a podiatrist who can properly evaluate your foot, and offer treatment options that are correct for you.
Stress fractures occur when there is a tiny crack within a bone. To learn more, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain free and on your feet.
How Are They Caused?
Stress fractures are the result of repetitive force being placed on the bone. Since the lower leg and feet often carry most of the body’s weight, stress fractures are likely to occur in these areas. If you rush into a new exercise, you are more likely to develop a stress fracture since you are starting too much, too soon. Pain resulting from stress fractures may go unnoticed at first, however it may start to worsen over time.
Risk Factors
- Gender – They are more commonly found in women compared to men.
- Foot Problems – People with unusual arches in their feet are more likely to develop stress fractures.
- Certain Sports – Dancers, gymnasts, tennis players, runners, and basketball players are more likely to develop stress fractures.
- Lack of Nutrients – A lack of vitamin D and calcium may weaken the bones and make you more prone to stress fractures
- Weak Bones – Osteoporosis can weaken the bones therefore resulting in stress fractures
Stress fractures do not always heal properly, so it is important that you seek help from a podiatrist if you suspect you may have one. Ignoring your stress fracture may cause it to worsen, and you may develop chronic pain as well as additional fractures.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Children's Feet are Different Than Adult's Feet

There are 26 bones in each foot, and they are designed in a complex way to support the body, absorb shock while walking and running, and conform to specific surfaces. When babies are born, their feet are mostly cartilage, which will harden into bones at approximately 13 years of age. The bones will develop gradually, and it is beneficial for them to wear shoes that fit properly when walking begins. Research has indicated the feet grow the fastest in the first three years, and may grow up to nine sizes during that time. Greater activity levels in children produce more stress in the feet than adults, and it is suggested that shoes which have extra cushioning be worn during the early years. Children’s shoes may show wear and tear faster than adult’s shoes, and this may be the result of excess sweating that occurs during physical activities. There are many choices to consider when purchasing children’s shoes, and it is advised that you speak with a podiatrist who can help you to make the right decision for your children’s feet.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Child's Feet
It is never normal for a child to experience pain in his or her feet. Foot pain that lasts more than a few days and limits a child’s ability to walk should be examined by a podiatrist. Many adult foot ailments originate in childhood and may be present at birth. Common foot issues that are experienced by children are pediatric flat foot, Sever’s disease, ingrown toenails, and plantar warts.
A child’s foot grows rapidly during the first year, allowing it to reach almost half of their adult foot size. Consequently, foot specialists consider the first year to be the most crucial point in the foot development process. There are ways you can help ensure that your child’s foot develops properly. One way is to carefully look at your baby’s feet. If you notice any deformities, you should immediately seek professional care. You should also loosely cover your child’s foot, since tight coverings may prevent movement and inhibit normal development. Another tip is to change the baby’s positioning throughout the day. If your baby lies down in one spot for too long, it may put an excess amount of strain on the feet and legs.
It is best that you try not to force a child to start walking. Children will begin to walk when they are both physically and emotionally capable to do so. You should also avoid comparing your child’s walking progress with other children because the age range for independent walking may range. When your child’s feet begin to develop, you may need to change both their shoe and sock size every few months to allow room for their feet to grow.
Kids are sometimes prone to splinters, cuts, and severe injuries because they tend to walk around barefoot. This also makes them more susceptible to developing plantar warts which is a condition caused by a virus that invades the sole of the foot through breaks in the skin. These ailments can be avoided by making sure your child wears shoes in unsanitary environments. You should also wash any minor cuts or scrapes on your child’s feet. It is a myth that exposure to fresh air will heal injuries; fresh air will only expose your child’s cuts to germs.
As a parent, you should ensure that your child’s feet are developing properly and are being properly maintained. Consequently, it is important that you perform routine inspections on his or her feet to detect any injuries or deformities in their early stages. Early detection and treatment will help to ensure that your child does not develop any serious foot conditions.
Hard and Soft Corns

Corns are spots that can form on the feet that are made up of thickened skin. Importantly, corns are distinct from warts and calluses. At their core, corns are hard and tough, yet are surrounded by skin that is inflamed. There are three different kinds of corns that may develop on your feet. The first is known as soft corns. This kind of corn primarily develops in between the toes of the feet. They might develop when friction occurs between the toes, typically caused by shoes with a small toe box. Soft corns also tend to be a white color. Soft corns are distinct from hard corns, the second kind of corn. Hard corns tend to develop on the flat, bony areas of the foot. In size, hard corns are both tiny and circular. A hard corn may develop in response to friction along with the inside of ill-fitting shoes. The third kind of corn is known as a seed corn, which can develop on the ball of the feet. Having corns may not seem consequential in some cases, but it is nothing to take lightly. Contact a podiatrist about your corns for treatment options.
If you have any concerns regarding your feet and ankles, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctors to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns: What Are They, and How Do You Get Rid of Them
Corns are thickened areas on the skin’s surface, to the point of being irritating and sometimes painful. Commonly found on the feet, corns are circular or cone-shaped. They develop where there are areas of pressure or friction, such as on the little toe when it rubs up against shoes, or on the ball of your foot.
Corns are often confused with a callus, but there is a difference between them. Corns can be raised bumps that are painful to the touch. They consist of a rough, thick area of skin that may be dry or waxy. Corns tend to be surrounded by skin that is inflamed, and are usually much smaller than calluses.
Removing the dead skin that has built up is the key in treating corns. Salicylic acid medication is most common in accomplishing this. The acid works by dissolving keratin, which is the protein that makes up the majority of corns. You can purchase salicylic acid over-the-counter in products such as wart removers. It comes in a variety of forms such as medicated pads, drops, or creams. However, people who are diabetic should not use salicylic acid, but should instead consult their doctor immediately.
According to the product directions, applying the medication directly onto the corn will treat it. The top layer of the corn will begin to turn white after use. When that occurs, the layers of skin can then be peeled away, making the corn smaller. Shaving off corns with razors or other pedicure equipment is never a good idea. This can lead to infection. If your corn gets infected, and is not treated immediately, a visit to the doctor will be necessary.
Another way to treat corns and help prevent their return is by using orthotic inserts, fitted by a podiatrist. Inserts fit right into your shoes and adjusts the way your foot fits into your shoes. This fixes the way you walk. This will lower your chances of getting corns, and eliminate current corns by reducing rubbing from friction.
Surgery is rarely used to treat corns, but does occur on occasion. Surgery actually deals with the underlying issue that causes corns. During surgery, the bone is shaved and any abnormalities are corrected, thus reducing the amount of friction that occurs during walking.
To prevent corns, the first step is reducing friction. Always wear shoes that fit well and don’t rub your feet. Pads can be purchased if you notice rubbing developing. These pads can be purchased over-the-counter, and can be simply placed on the irritated area. Wearing cushioned insoles in your shoes can always reduce the friction, and making sure to wear well-fitting shoes. This will ensure that your foot is not being squeezed awkwardly, and prevent corns from forming in the first place.
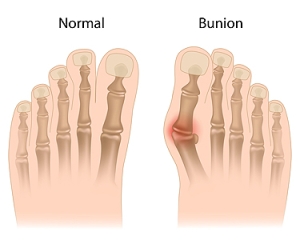
Understanding Bunions
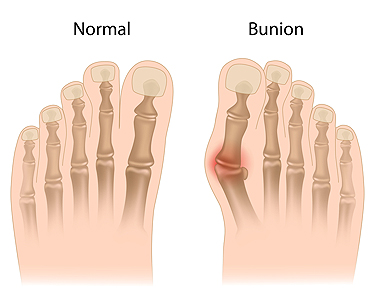
Bunions are a foot deformity caused by a misalignment of bones that connect at the joint of the base of the big toe. This deformity causes a bony protrusion at this joint, which then causes the big toe to lean toward the other toes, rather than pointing straight forward. Certain factors can make a person more likely to develop a bunion, such as wearing high-heeled shoes regularly, overpronating, and having certain genetic factors, loose ligaments, or other anomalies in foot structure. Aside from having an irregular appearance, a bunion can cause pain, swelling, numbness, or burning in the big toe joint and/or in the first metatarsal bone (in the forefoot). It may also be difficult to walk or find shoes that fit. It is a good idea to begin treating a bunion as soon as possible for the best results in correcting it. If you already have a fully developed bunion, or believe one is forming, make an appointment with your podiatrist for an examination and evaluation.
If you are suffering from bunion pain, contact one of our doctors of Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Are You Suffering From Ingrown Toenails?
Where Is the Plantar Fascia?

The condition plantar fasciitis exists when the plantar fascia becomes inflamed. It is the band of tissue that is found on the bottom of the foot that can become torn or damaged from a foot injury. Additionally, it may happen from standing for most of the day, or from frequently walking on hard surfaces. Many people experience general foot pain with plantar fasciitis, and the foot may feel stiff and tender. It is beneficial to adjust daily living activities, and to temporarily stop doing what caused the pain. There are patients who find mild relief when specific foot exercises and stretches are performed, in addition to possibly wearing orthotics in their shoes. In severe cases, surgery may be a necessary option to repair the damaged portion of tissue. If you have heel pain, please confer with a podiatrist who can properly diagnose plantar fasciitis, and offer you correct treatment advice.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our doctors from Kitsap Foot & Ankle Clinic. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact one of our offices located in Bremerton and Port Orchard, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.